10 Things You Should Know About Cataracts

If you’re in your late 50s and you begin to have blurred or cloudy vision, as if you’re looking into a frosted glass, you might have a cataract.
You are born with a clear lens that allows you to focus your eye. Cataracts cloud the eye’s lens, which typically targets older adults. While cataracts are common as we age, if it’s left untreated, they can lead to blindness.
In this blog, we’ve rounded up ten facts about cataracts and cataract surgery you should know.
1. 95 percent of seniors in Singapore have cataracts
Cataracts are the leading cause of blindness, responsible for half of the 40 million blind people in the world. Each year, 5 million new cases of cataract blindness are reported. In fact, there are more cases of cataracts worldwide than there are other severe eye conditions like diabetic retinopathy, glaucoma, and macular degeneration combined.
In Singapore, about 95 percent of the population over 70 years old, and 80 percent of those over 60, have cataracts. Unfortunately, this eye condition is common. Hence, it’s only fitting you know the risks involved before it compromises your vision.
So, what is a cataract, and how does it form? Inside the eye is a transparent structure called a lens, which can change its shape to allow the eyes to shift their focus on objects. Usually, the lens is clear, but when a cataract forms, you’ll have blurry and cloudy vision.
The good thing is this eye condition is treatable. Getting a routine eye exam is crucial to detect any abnormality early. This way, adverse complications can be averted.
2. There are three types of cataracts
Cataracts form when protein builds up in the lens of your eyes, making them cloudy. Though it’s a common eye condition, it has many types.
- Nuclear sclerotic cataract. Also called nuclear cataracts, it is the most common type , affecting many older adults. Nuclear means the centre of the lens, while sclerotic refers to the hardening of the lens. This type of cataract develops over time and can cause yellowing and hardening of the centre of the lens.
- Cortical cataract. This type of cataract develops around the outer layer of the lens called the cortex. It gradually reaches the centre part of the lens, which makes the light that enters the eyes scatter. As a result, you’ll experience glares, blurred vision, and contrast and depth perception problems.
- Posterior subcapsular cataract. This cataract occurs at the back part of the lens, affecting your reading and night vision. It usually starts as a tiny cloudy or opaque area on the rear surface of the lens. However, this is the fastest to progress compared to the other types.
Read: Cataracts: Unblurring the Facts
3. Blurry vision is the most common symptom of cataract
Cataracts in the early stages start as small and may have little effect on your vision. However, as the condition progresses, you may develop blurry vision, the most common symptom of cataracts.
Your vision may become cloudy and blurry. Over time, as cataracts worsen, less light reaches the retina, which may affect night vision. Other cataract symptoms you may experience include glare around bright lights, halos, distortion of vision, dull colours, dimmed vision, double vision, and the frequent need to change eyeglasses due to progressing nearsightedness.
4. Cataracts can lead to blindness if left untreated
Cataracts often begin to develop as you get older. Over time, cataracts worsen and start to interfere with vision. As a result, you may find it challenging to perform tasks like working, reading, and driving, to name a few.
If it’s left untreated, it can cause blindness. A cataract is the most treatable type of eye condition. The good thing is cataract surgery is effective in treating cataracts and restoring your vision.
In this procedure, the surgeon removes the defective and diseased lens and replaces it with an artificial one. Along with other supportive interventions, such as prescription glasses, cataracts can be managed if spotted early.
5. Cataract surgery is the only proven treatment for cataracts
If your vision gets cloudy because of cataracts, your doctor may suggest cataract surgery to remove the defective lens. It’s a safe and most commonly performed surgical procedure. Although you’re awake while the eye doctor performs the surgery, you’ll be given a calming medication to mildly sedate you and special numbing eye drops or gel so you won’t feel any pain or discomfort during the procedure.
There are three types of cataract surgery:
- Phacoemulsification. This is the most common procedure to remove a cataract in the eye. It utilises a unique pen-shaped instrument to break up the cloudy lens. To do this, the surgeon will insert the probe into the lens through a small incision at the edge of the cornea. Next, an ultrasound probe breaks up the cataract to easily remove it. After the natural lens has been removed, it is replaced by an artificial lens, called an intraocular lens (IOL) — a clear, plastic lens that eventually becomes a permanent part of the eye.
- Extracapsular cataract extraction (ECCE). Also known as modern cataract surgery, ECCE involves removing a circular anterior portion of the lens capsule. It removes the cataract in one piece through a larger incision, leaving the elastic capsule covering the lens. As a result, it allows the implantation of the IOL. The primary purpose of this surgery is to restore clear vision.
- Laser-assisted cataract surgery. This cataract surgery involves using a laser to open the capsule and soften the cataract. Then, an ultrasound device or camera is used to guide the surgeon through a 3-D surgical plan. At the same time, data is transmitted to a computer to determine the cataract’s size, location, and depth.
You have many choices regarding the type of cataract surgery, but all these are the same regarding success and safety.
Remember, there’s no other way to treat cataracts besides surgery. If it’s detected early, the doctor can suggest preventive measures to slow down its progression. However, if there’s blurred or cloudy vision, surgery is necessary.
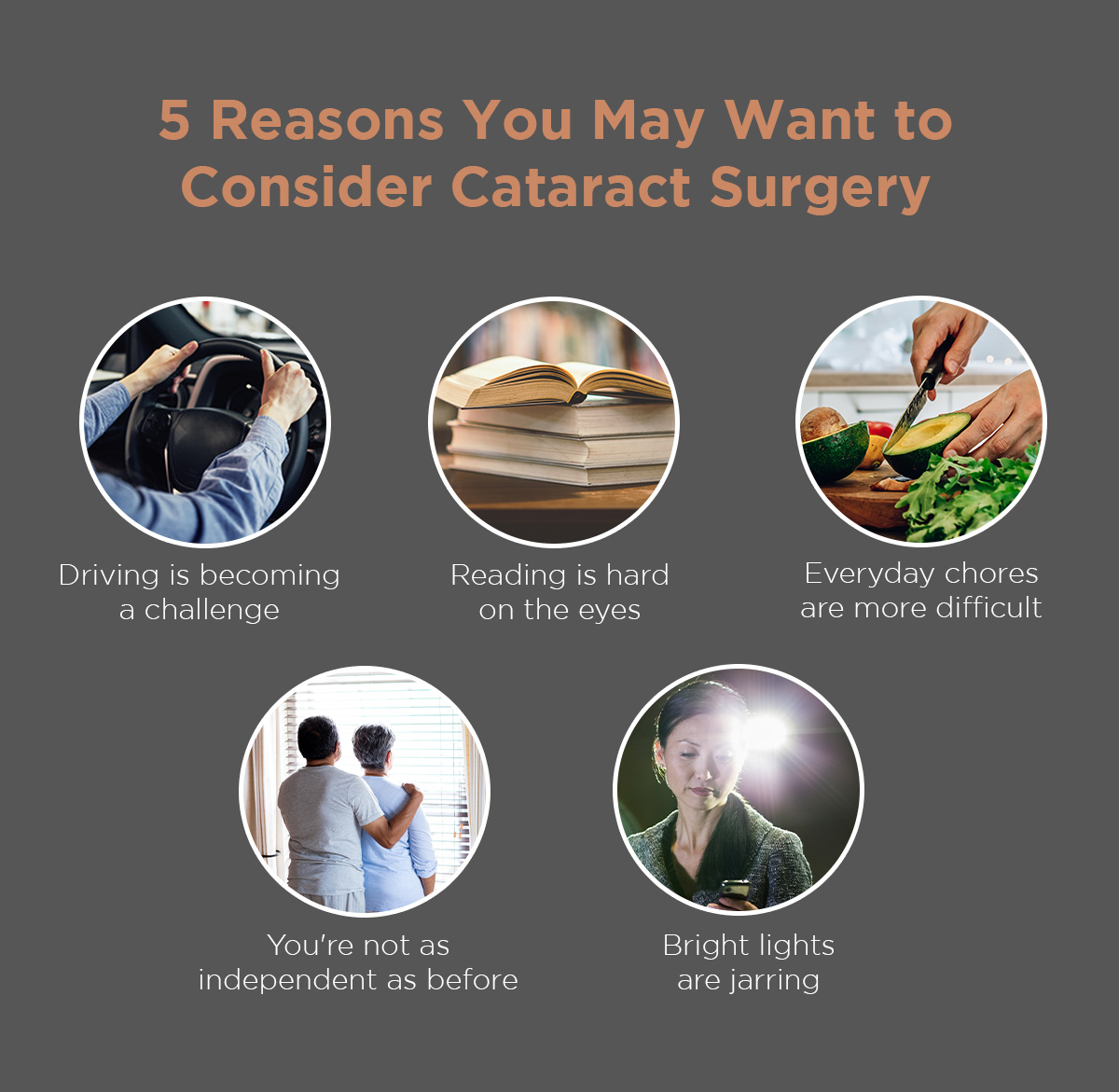
When considering cataract surgery, ask yourself these:
- Can you safely drive or perform tasks?
- Do you have problems reading or watching television?
- Is it difficult to cook, do yard work, or do house chores?
- Do vision problems affect your level of independence?
- Do bright lights make it more difficult to see?
6. Most people develop clearer vision within 24 hours of surgery
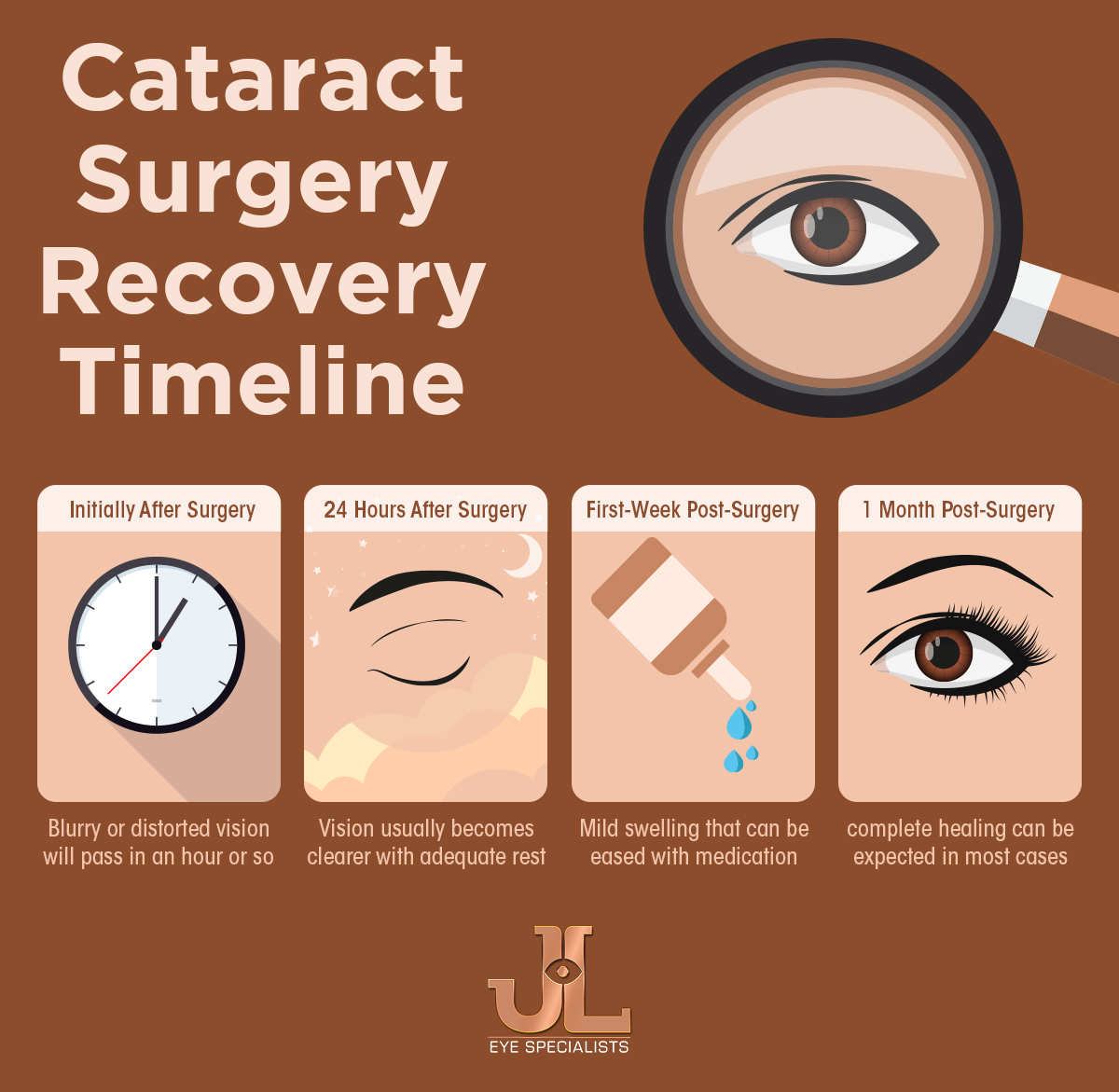
After cataract surgery, blurry vision is expected immediately after the procedure. It typically clears within 24 hours of surgery and up to two to three days.
What to expect after surgery? Since you were used to brown-tinted or yellowish vision due to cataracts, you may notice that colours may seem brighter after the procedure.
You must wear an eye shield on the operated eye. It will protect your eye from touching and infection. After that, the doctor will prescribe eye drops and medications to reduce inflammation, control eye pressure, and prevent contamination or infection.
Further, you may feel mild discomfort and itching for a few days following surgery, but it’s normal and will go away. Though your vision will improve over the following days, you may experience some side effects, including grittiness, sensitivity to light, double vision, and watering.
In addition, you need to take care of your eyes after surgery. Avoid lifting heavy items because it can cause elevated pressure in the eyes. It can interfere with healing, and worse, it can damage the eye. Also, avoid strenuous activities for about a week after surgery, which includes running, golf (if carrying heavy caddy bags), basketball, hill walking, heavy gardening, and childcare for children who need lifting.
Other activities that can raise intraocular pressure include reaching up high or bending below your waist. Plan out your movements around the house, and ask for assistance from your family to perform tasks. Again, it’s important to prevent straining yourself.
About a month after surgery, most people are completely healed, as long as post-operative instructions are followed. Follow-up consultations are essential for your doctor to evaluate your recovery progress. This will also pave the way to determine if there are complications. From there, routine eye check-ups are recommended to ensure your vision is clear and no new cataract formation has occurred.
Read: Cataract Surgery Recovery Timeline
7. Age is not the only factor for developing cataracts
Most cataracts progress slowly over time because of ageing and can affect those over 50. However, some cases are seen among infants and young children due to medicines or trauma.
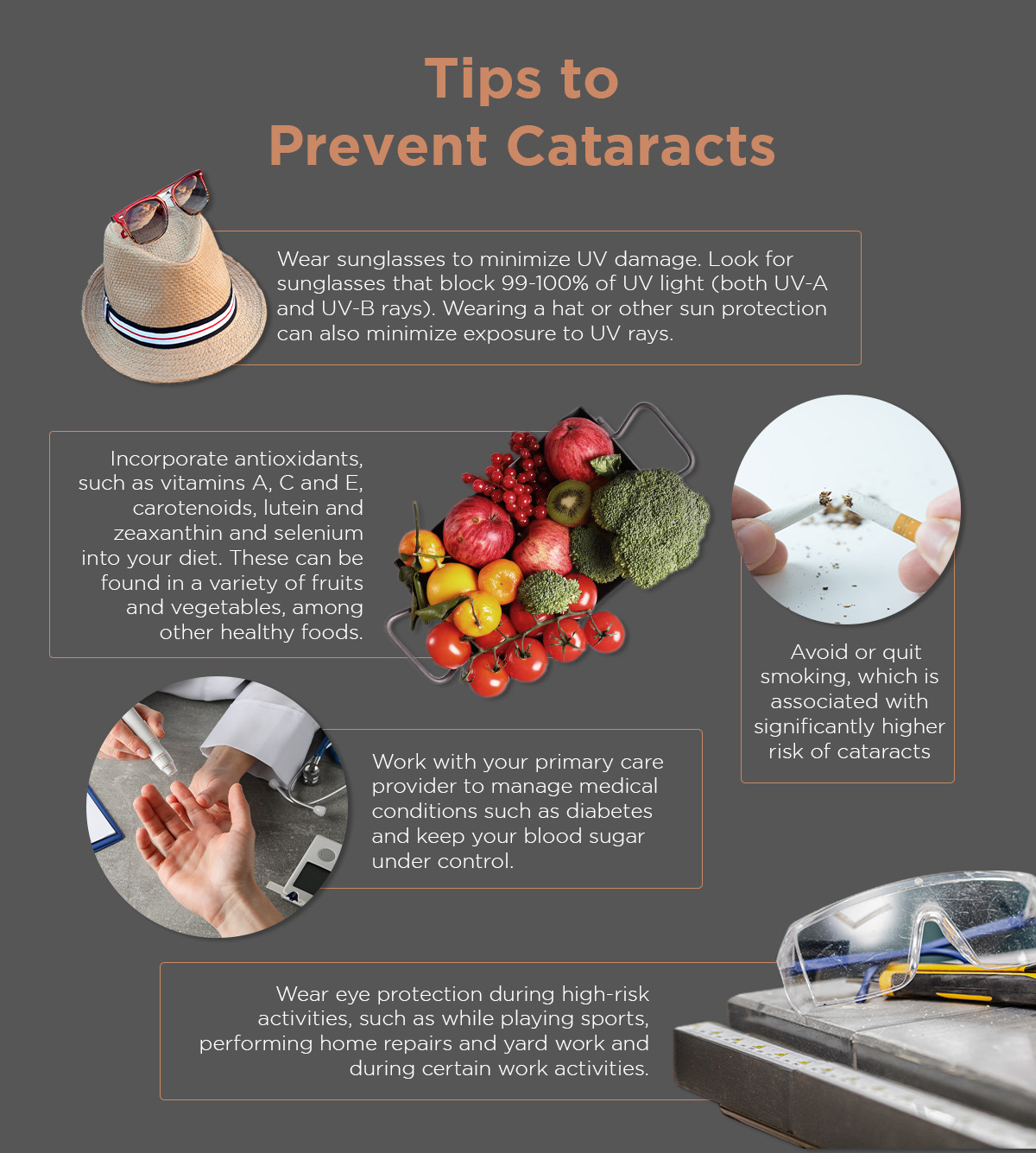
Common cataract formation risk factors include chronic smoking, excessive alcohol intake, ultraviolet ray exposure, and family history of cataracts. Diabetes, eye trauma, steroid use, radiation therapy, and phenothiazine can all hasten cataract formation and progression.
In most age-related or senile cataracts, the condition progresses gradually over the years. However, in people with comorbidities, like those with diabetes, the cataract progresses rapidly over a short time.
Meanwhile, trauma-related cataract is a fast-growing condition that can develop within weeks of injury to the lens. It occurs when the fibres in the lens become damaged and disrupted. The most common injury causes include radiation exposure, chemical exposure, and penetrating or blunt trauma.
8. Although cataract surgery is among the safest, there can be complications
Complications after cataract surgery are uncommon, and most can be treated effectively. However, every surgical procedure has risks and complications.
Inflammation and infection. Surgical procedures involve incisions that can be infected. Germs can get into your eyes during surgery. At the same time, swelling and redness may occur after surgery, but if it’s severe, you need to see your doctor.
Bleeding. One of the complications of cataract surgery is suprachoroidal haemorrhage, which occurs in people with hypertension, diabetes, and other existing health problems. This is rare but requires emergency medical attention to avoid permanent vision loss.
Retinal detachment. The retina is found at the back of the eye. After cataract surgery, there is a risk that it pulls away from the tissues supporting it. It’s a medical emergency that can cause blindness if not managed immediately. The symptoms of retinal detachment include blurred vision, flashes of light, reduced peripheral vision, the sudden appearance of floaters, which are specks that seem to float through your vision, and a shadow that curtains over your vision field.
Macular oedema. This is usually caused by the buildup of fluid in the macula, the central part of the retina.
Dislocation of the intraocular lens. This happens when the lens implant isn’t correctly seated in the eye’s capsular bag. In some instances, it can become dislocated. The common symptoms include seeing the edge of the lens and double vision. Though this rarely occurs, immediate surgery to correct it is needed.
Posterior capsule opacification (PCO). May happens in 14 to 60 percent of uncomplicated cataract surgeries. This occurs in people with prior eye surgeries, diabetes, and eye problems that form small particles or transparent bubbles called Elschnig’s pearls, which are trapped behind the lens.
The doctor will monitor and advise you to watch for warning signs of severe complications. These include decreased vision, very red eyes, severe pain, floaters or discharge from the eye.
9. Patients still need glasses after surgery
Innovations in cataract surgery have enabled patients to achieve clear vision, and most may not use eyeglasses. However, some patients with refractive errors who are not compatible with the intraocular lenses they chose still need glasses after surgery.
The lens you and your surgeon choose to implant during surgery plays a huge part in your need for glasses.
10. Cataract surgery is consistently improving
There are three types of intraocular lenses—monofocal, astigmatic or toric, and multifocal.
The monofocal lenses are the most commonly used ones, allowing you to correct nearsightedness or farsightedness. However, in this IOL type, you may still need glasses for tasks like driving and reading.
On the other hand, astigmatic or toric lenses allow you to correct for far or short distances while correcting astigmatism. Multifocal lenses will enable you to see short and far distances.
Other lens technology options include trifocal, extended depth focus (EDOF), and Eyhance lenses. A trifocal lens has one corrective zone stretched to allow intermediate and distance vision. An EDOF lens can correct intermediate vision, distance vision, and near vision in patients with presbyopia. Meanwhile, the new development in IOL technology is the Eyhance lens, which increases the depth of focus compared to monofocal lenses, making you see far objects clearly and improving your intermediate, allowing you to do more tasks even without eyeglasses.
Customised intraocular lens technology, available for all refractive needs, is vital to achieve comfort after cataract surgery.
Read: Refractive Options During Cataract Surgery
The Takeaway
Cataracts can be debilitating if left untreated. Fortunately, treatment options and advances in cataract surgery are available to help restore clear vision. Aside from routine eye exams, it would help if you visited your doctor for diagnostics and evaluation.
At JL Eye Specialists, we offer a full range of intraocular lens technology available for your refractive needs. Please book a consultation with our medical director Dr Jimmy Lim so that he can create a tailored treatment plan for you.
Related Post:
More Topics to Explore:
Relevant Services:
Our Doctor

DR. JIMMY LIM
Dr. Jimmy Lim is a top ophthalmologist for cataract eye surgery in Singapore, offering over 20 years of expertise in cataract treatment and management.
Gleneagles Medical Centre
6 Napier Road #07-10,
Singapore 258499
Phone: +65 6258 8966
Fax: +65 6258 8766

JL Eye Specialists is an ophthalmology clinic in Singapore that specialises in general ophthalmology, cornea, refractive (LASIK), and cataract surgery.
To cover the expenses that you may incur, we accept several corporate and international insurance policies. If you have any of the insurance plans at this side, please let us know when you schedule an appointment with us. For more questions, feel free to contact us at +65 6258 8966.